Can’t Sleep? Check Your Sex Hormones
The inability to fall asleep, or stay asleep, is very common, and so much so that we may look for a quick fix in the form of melatonin or a sleeping drug to help us get a restful night’s sleep. Anti snoring devices can help snorers sleep better, but many other factors affect sleep as well.
Unfortunately, while that may work at the moment, sleep issues are our body’s way of saying that something is not quite right. Much like our sleep/wake cycle, sex hormones (estrogen, progesterone, and testosterone) follow a cycle and when not in the proper rhythm, can affect our sleep by altering mechanisms that would otherwise allow us to have a quality night’s sleep.
Sex hormones are derived from cholesterol, made in the adrenal cortex (two glands that sit on top of each kidney also responsible for blood pressure and our stress hormone, cortisol), and reproductive organs (testes in men, ovaries in women). Fat cells are responsible for making estrogen, as well as an enzyme that turns testosterone into estrogen.
Low testosterone has become increasingly common in men over the past few decades and can contribute to symptoms such as poor sleep, obesity, anxiety and depression, low energy, low libido, and gynecomastia.
In women, elevated testosterone has also become more prevalent (e.g., polycystic ovarian syndrome) and has symptoms like insulin resistance, extra hair growth, and menstrual irregularities. However, both men and women in these scenarios are also likely to have elevated estrogen, which directly impacts sleep by inhibiting melatonin, our sleep hormone.
Moreover, insomnia can be the first sign of perimenopause in women due to hormone fluctuations (progesterone plummets faster than estrogen, so an increased ratio), that may be a contributing factor to hot flashes.
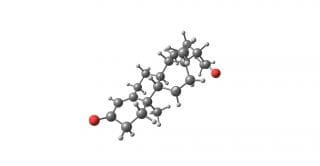 Estrogen is made from testosterone by the enzyme aromatase and added into our body through the way of stress, grains, dairy, alcohol, smoking cigarettes, blood sugar issues, and chemicals in beauty, cleaning and skin care products that mimic estrogen. Fat cells make estrogen and secrete an enzyme called aromatase that converts testosterone into estrogen.
Estrogen is made from testosterone by the enzyme aromatase and added into our body through the way of stress, grains, dairy, alcohol, smoking cigarettes, blood sugar issues, and chemicals in beauty, cleaning and skin care products that mimic estrogen. Fat cells make estrogen and secrete an enzyme called aromatase that converts testosterone into estrogen.
Additional factors that can raise estrogen stem from stress (e.g., mental/emotional, untreated concerns, poor diet, sedentary lifestyle) that shunts resources derived from vitamin D and cholesterol into pathways that make cortisol instead of our sex hormones. Many of the lifestyle habits mentioned above add extra strain on the liver’s detoxification systems.
The liver is the main organ responsible for binding up and detoxing excess estrogen, as well as testosterone, progesterone, and cortisol, and responsible for over 500 processes. On a side note, estrogen doesn’t always have to be out of range on any test, as normal estrogen levels can be high if testosterone and progesterone are very low.
Too much estrogen can affect other organ systems such as our thyroid by increasing a protein that binds up the thyroid hormone (and slows down metabolism- another hindrance when we want to lose weight).
Estrogen also disrupts gut bacteria that also helps excrete excess, inhibiting melatonin (our sleep hormone), and contributing to sugar and carbohydrate cravings by making our cells more resistant to insulin (what takes glucose into our cells for energy).
While estrogen now seems like a likely culprit, we are caught in a ‘chicken and egg’ scenario, as a poor diet can also be a stressor on the body (stress also inhibits thyroid hormone, which can slow down bowel movements and allow toxins to get reabsorbed) contributes to weight gain and inadequate gut health, amongst other issues.
Not sleeping well alters hormone balance as most hormones get produced at night, and a more sedentary lifestyle can add extra pounds, which correlates to extra hormones. Anxiety and depression may have some organic cause too as estrogen is broken down by an enzyme called catechol-o-methyltransferase (COMT), the same enzyme responsible for breaking down more excitatory neurotransmitters like dopamine and epinephrine (as well as certain drugs and foreign substances).
If there’s not enough to go around, then neither estrogen nor these neurotransmitters can get broken down to appropriate levels. And typically anxiety and depression aren’t in the recipe for what it means to get good, solid sleep.
 There is hope for balancing hormones and sleeping soundly! Hormones are wonky, pulsatile, and quite volatile yet fortunately, the many ways we can help balance them are ways we can also improve sleep. Focusing on dark leafy green vegetables (e.g., kale, spinach, chard) and cruciferous (e.g., broccoli, cauliflower, brussels sprouts) are packed with many vitamins and minerals needed to make and metabolize hormones, as well as fiber that helps feed good gut bacteria.
There is hope for balancing hormones and sleeping soundly! Hormones are wonky, pulsatile, and quite volatile yet fortunately, the many ways we can help balance them are ways we can also improve sleep. Focusing on dark leafy green vegetables (e.g., kale, spinach, chard) and cruciferous (e.g., broccoli, cauliflower, brussels sprouts) are packed with many vitamins and minerals needed to make and metabolize hormones, as well as fiber that helps feed good gut bacteria.
Cruciferous vegetables, in particular, have a sulfur compound that helps turn estrogen into one of it’s more protective metabolites, as well as bind up extra estrogen. Healthy fats are a must, as fats are the building blocks of hormones, and also help diminish cravings, improve weight loss efforts, and improve moods, such as through nutrients found in avocado, nuts, wild salmon, olive oil, and coconut oil. Magnesium (also knows as ‘nature’s relaxer’) is also an important mineral, found in foods like nuts and avocados, and through Epsom salt baths! Aiming for bedtime before 10:30 pm optimizes our melatonin production (our most potent endogenous antioxidant) and helps prevent that ‘second wind’ that usually happens around 11 pm.
Working with a knowledgeable practitioner can further help guide and prioritize treatments and tests, especially when considering herb/drug/nutrient interaction, as well as what tests to order. Fortunately, even being able to work these tips into your lifestyle adds high value as it also doubles as preventative care.

